 kaiserpapers.com/businesspractices
kaiserpapers.com/businesspractices
Permanente Medicine: A Conversation With Jed Weissberg, MD, On Defining Permanente Medicine
(Jed Weissberg, MD, is the Associate Executive Director for Quality and Performance Improvement at The Permanente Federation, where he has led efforts to better understand the meaning of Permanente Medicine. Before joining the Federation in February 1998, Dr Weissberg served as PIC at the Fremont Medical Center in Northern California. Interview conducted by TPJ Communications Editor, Jon Stewart.)
The Permanente Journal: Dr Weissberg, when you joined The Permanente Federation, one of the first things you did was initiate a systematic approach to defining and talking about Permanente Medicine. Why was that such a priority for you?
Jed Weissberg, MD: Actually, I'd never heard of Permanente Medicine before I came to the Federation. But Jay Crosson (Executive Director of The Permanente Federation) and everyone else there was talking about "Permanente Medicine" and "Permanente Practice" as if it were common knowledge. So after about a week, I finally got up the courage to ask Jay, "What's this thing you call Permanente Medicine?"
Well, it turned out he had a very clear idea in his own head of where this all went, but he was thinking mostly in terms of the structural and accountability issues inherent in the Permanente Medical Groups--things like self-governance, self-management, and group responsibility. Those are the essential principles by which Permanente Medical Groups have organized themselves and held themselves accountable, and they really do seem to define what's unique about the way we organize ourselves. But when some of us sat down and tried to flesh out those concepts in terms that would have a more emotional reality, we realized that there had to be another side of the picture, one that represented the clinical and patient side in addition to the organizational qualities. And that's what we've come to call the "performance principles" of Permanente Medicine--quality medicine, the Permanente-Patient relationship, and resource management. These concepts, of course, are all interrelated.
TPJ: Why is it important to articulate these principles? Haven't they been operative all along without a formal definition?
JW: Well, remember that Sidney Garfield, who started this whole thing, defined what he thought was unique about the Permanente way of organiz ing and delivering medical care. We're all familiar with those elements--what we call the "genetic code"--things like prepayment, group practice, prevention, comprehensive coverage, and physician responsibility for medical care. But as the program expanded into new regions, various medical groups started introducing variations on themes in terms of incentives and approaches to care and their own kinds of delivery systems. I think we still had the impression that we were basically different from everyone else and similar to one another, but it was getting harder to articulate that that was the case. It may be true that for a long time it didn't really matter, but by the 1990s, when everyone else was trying to do "managed care," we got to the point where we really did need to differentiate ourselves from all the rest of managed care, which was taking such a bashing in the press. That meant that we needed to have a clearly defined identity. We needed to really understand among ourselves--and then communicate to others--what it is that makes us different.
 Jed
Weissberg, MD, uses the Permanente Map to define Permanente Medicine to
a group of Permanente physicians. (See map and related
story.)
Jed
Weissberg, MD, uses the Permanente Map to define Permanente Medicine to
a group of Permanente physicians. (See map and related
story.)
TPJ: It wasn't just the mass media doing the bashing. The professional press was attacking some of the underlying principles of Permanente Medicine, as well.
JW: Yes, like those articles in the New England Journal that were criticizing the so-called "distributive ethic" of prepaid group practices. They were saying basically that physicians could not provide optimal care for each of their individual patients and for the entire population of patients under the group's care at the same time. They implied that prepaid group practice physicians had become "double-agents," acting on behalf of the health plan, or of third-party payers, instead of on behalf of their patients. And they were saying that population-based care means deliberately providing poorer care for some patients than for others.
These were very powerful messages, coming from a powerful professional journal, and they went to the very heart of Permanente Medicine, the ethic of prepaid group practice. So, in some ways, what we were doing in trying to articulate the principles of Permanente Medicine was to restate our claim to professionalism around a core set of ethical beliefs. I suppose it was not unlike the challenge that Garfield and the other pioneers of Permanente Medicine faced from organized medicine back in the 40s and 50s.
TPJ: It's interesting that this initiative also came about at a time when the medical groups were reorganizing themselves at the national level vis-à-vis the health plan. Was that relevant?
JW: I think so. This new emphasis on understanding the uniqueness and the strength of Permanente Medicine coincided with the creation of the Federation, which had enabled much more interaction among the medical groups throughout the program than had ever before existed. And I think the Permanente leadership saw that there were actually some pretty significant differences among the regions in the ways they were delivering care--especially in some of the regions that were having difficulty. This naturally made the leadership want to figure out what was working and what wasn't. And of course much of the weakness was in areas where the delivery system was at variance with the principles that made us strong in our core markets. There was a sense of needing to get back to first principles--but first to figure out what they were.
TPJ: That was also a time when the leadership in Oakland was developing what is now known as the KP Promise, or brand strategy, which puts a lot of emphasis on positioning KP as a high-quality, service-oriented delivery system. Is the KP Promise compatible with Permanente Medicine?
JW: Very much so, fortunately. Because I think the KP Promise, with its focus on quality medicine, really did grow out of an understanding of the organization's traditional strength, which is the physician-directed delivery system. The KP Promise includes that notion of physician responsibility, which is at the heart of what we call "group responsibility" and "self-management" in Permanente Medicine. And the Promise is also built around the performance side of the Permanente Medicine paradigm, with its emphasis on quality medicine. In fact, in some ways, the KP Promise might be said to represent the third, invisible side of the Permanente pyramid, with the structural principles and the performance principles on the other two sides. What is different about the Promise is that it incorporates perspectives that have not been articulated as aspects of Permanente Medicine, such as the essential role played by our employees and the interests of KP members. The Promise blends those interests more explicitly than the principles of Permanente Medicine, which are more self-reflective from the medical group point of view.
TPJ: What was the process you followed in identifying and defining the principles of Permanente Medicine? How much input did you get from beyond the 27th floor (the Federation Executive Offices in the Ordway Building in Oakland)?
JW: A lot, ultimately, and we're still working at it. But it needs to be said that Jay Crosson and a handful of Federation staff people did a lot of the early conceptual work, and most of it has stood up under pretty intense reexamination--especially those three structural principles that Jay identified: group responsibility, self-governance, and self-management. People will argue about the exact labeling, but there's a lot of consensus around the meaning. And, of course, even those principles were really an outgrowth of elements of the genetic code, so the debt goes back to Garfield.
What I started doing was collecting a lot of mission statements, orientation materials, and strategic plans that various PMGs had worked on, where they had tried to identify basic principles of practice. The Colorado PMG had a very well thought out set of principles, and so did some others, like Georgia. It was surprising how similar those principles were, even though the groups had never shared them before. So we tried to identify the common threads among them and then feed them back to regional leaders and various reactor groups, including the Permanente Executive Committee and the day-long Permanente Medicine roundtable discussion in Colorado, where virtually every PMG was represented (see "Permanente Medicine Roundtable" article).
Over the last couple of years, between Jay Crosson and myself and a few others, we've talked to dozens of groups--mostly physician groups--about Permanente Medicine. Every time we do it, the definition takes on a little more clarity. We keep testing it and looking for ways to make the definitions operationally useful, such as in the performance analysis and improvement work we do. And, so far, we've gotten remarkably positive feedback. People really like to talk about it, I think because it provides a common language for understanding some very complex ethical issues that are common to all of us.
TPJ: It's easy to see how this work can be useful in terms of differentiating KP from the bad guys of managed care in the public arena, but how is it useful internally and operationally? How does it relate to the day-to-day provision of medical care?
JW: What these principles do is give us a framework for holding ourselves accountable to one another and to our patients for the things we say we believe in. If these principles really define our professional beliefs about the best way to provide health care, then we need to translate them into objective measures of accountability. We need to be able to say, "We practice what we believe in, and here's the data to prove it." So a lot of the work of defining Permanente Medicine has been defining objective measures for each of the principles, especially the performance principles around quality and resource management, but also the structural principles like self-governance and self-management. Do we really govern ourselves through representative leadership and due process? Does every PMG have the appropriate structures and processes in place for self-management and resource management? And can we point to appropriate outcomes measures as evidence of our accountability?
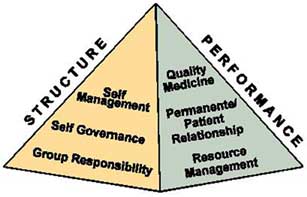 Figure
1. The Permanente Pyramid: The Principles of Permanente Medicine
Figure
1. The Permanente Pyramid: The Principles of Permanente Medicine
Remember, the medical directors of all the PMGs have agreed to hold one another mutually accountable for all performance--clinical, service, everything. That agreement really gave new meaning to the notion of "flying the Permanente flag." If we're going to call ourselves Permanente Medical Groups, that has to mean something specific and measurable, and Permanente Medicine gives us the conceptual framework for developing those specific measures. This part of the work is now in the hands of a number of national and interregional work groups, such as the KP Performance Review Committee, which recommends performance measures to the KP Partnership Group, the organization's top management group. The Care Experience Council is doing another key part of the work, focusing on measures of access and service.
TPJ: Those groups are all joint Permanente-Health Plan groups. But apart from that connection, where does KFHP fit into Permanente Medicine? Or doesn't it? Can you have Permanente Medicine without Kaiser Foundation Health Plan?
JW: That question borders on treason. But thanks for asking it, anyway. Because in all truth, you're not the first. It's a legitimate question that's worth exploring. However, in our current conception, KFHP has been an integral part of our understanding of Permanente Medicine ever since we started looking at it. Before I ever got involved, Jay Crosson talked about the principles of Permanente Practice existing within the context of an exclusive partnership with a not-for-profit health plan, and around here that means KFHP. Without that partnership, it's hard--maybe not impossible, but much harder--to imagine how Permanente Medicine could stand alone. I think the partnership adds a lot to the overall equation that makes up Permanente Medicine.
Related Permanente Medicine Articles:
The Priciples of Permanente Medicine
The Permanente Medicine Roundtable: Defining our Practice Principles
The Permanente Medicine Map
.
Back to kaiserpapers.com/businesspractices