
Kaiser Diagnostic and Treatment Documents
KAISER PERMANENTE CLINICAL PRACTICE GUIDELINES FOR EVALUATING ACUTE CORONARY SYNDROME IN CHEST PAIN PATIENTS IN THE EMERGENCY DEPARTMENT
 KAISER
PERMANENTE
KAISER
PERMANENTE
The Permanente Medical Group Clinical Practice Guidelines have been developed to assist clinicians by providing an analytical framework for the evaluation and treatment of selected common problems encountered in patients.
These guidelines are not intended to establish a protocol for all patients with a particular condition. While the guidelines provide one approach to evaluating a problem, clinical conditions may vary significantly from individual to individual. Therefore, the clinician must exercise independent judgment -and make decisions based upon the situation presented. While great care has been taken to assure the accuracyof the information presented, the reader is advised that TPMG cannot be responsible for continued currency of the information, for any errors or omissions in this guideline, or for any consequences arising from its use.EVALUATING ACUTE CORONARY SYNDROME IN CHEST PAIN PATIENTS IN THE EMERGENCY DEPARTMENT CLINICAL PRACTICE GUIDE LINES TEAM
CLINICAL LEADER Christina Shih,MD, Emergency, San Francisco
CPG TEAM Robert Cooper; MD, Cardiology, Oakland Carl Corrigan, MD, Medicine,Sacamento Robert Heller; MD, Cardiology, Hayward PamKotler; PhD, Department of Quality and Utilization* Eliot Mah, MD, Medicine, Sacramento Bill Plautz, MD, Emergency, South San Francisco David Yoon, MD, Emergency, Santa Clara
*Currently affiliated with the Institute for HealthPolicy, University of California, San Francisco and California Medical Review Inc.
PROJECT MANAGEMENT Jay Krishnaswamy, MBA, TPMG Department of Quality and Utilization
Linda Rogers, MPA, TPMG Department of Quality and Utilization
DATA ANALYSIS Helen Xu, MS,TPMG Department of Quality and Utilization
REVIEWERS Adria Beavel; RN, BS, Cardiology, South Sacramento Ralph Brindis, MD, MPH, Cardiology, San Francisco Tim Baker; MD, Emergency, Hayward James Cadden, MD, Emergency, Santa Rosa Uli Chettipally, MD, MPH, Emergency, San Francisco Edward Fischer; MD, Cardiology, South San Francisco Paul Feigenbaum, MD, Medicine, San Francisco TonyFiorello, RN, Assistant Manage Emergency, SantaRosa David S. Gee, MD, Cardiology, Walnut Creek Mateo Go Jr, MD, Cardiology, Santa Teresa Eric M.Koscove, MD, Emergency, Santa Clara Sushil Karmarkel; MD, Cardiology, Walnut Creek Eleanor Levin, MD, Cardiology, Santa Clara Philip Lee, MD, Cardiology, Santa Clara John Metcalf, Lab Dinector, Hyward Robert Mooney, MD, Emergency, Walnut Creek Roy Meyer; MD, Medicine, Santa Rosa Stanley J. Nussbaum, MD, Cardiology, Santa Rosa Michael A. Petru, MD, Cardiology, San Francisco Pankaj Patel, MD, Emergency, Sacramento Steve Rose, MD, Cardiology, South Sacramento William J.Raskoff, MD, Cardiology, San Francisco James Scillian, MD, Pathology, Stockton Richard Wakamiya, MD, Emergency, South Sacramento https://kaiserpapers,org/cajue/evalcoro/ Vincent Yap, MD, Medicine, Richmond
DESIGN & PRODUCTION
Gail Holan/Curvey
Ratified by the Operations Management Group and the Quality Oversight Committee KPNC Clinical Practice Guidelines can be viewed on-line on the Kaiser Permanente Northern California intranet website at http://clinicaMibrary.ca.kp.org. This website is accessible only from the Kaiser Permanente computer network. ãCopyright 1998 The Permanente Medical Group, Inc. All rights reserved. Please contact TPMG Department of Quality and Utilization at 510-987-2309 or tie-line 8-427-2309 for permission to reprint any portion of this publication. For additional copies of the guidelines, please call 510-987-2950 or tie-line 8-427-2950 or send an e-mail message to Clinical.guidelines@ncal.kaiperm.org.
CLINIAL PRACTICE GUIDELINES FOR EVALUATING ACUTE CORONARY SYNDROME IN CHEST PAIN PATIENTS IN THE EMERGENCY DEPARTMENT CONTENTS
INTRODUCTION Page 2
OVERVIEW OF CLINICAL PRACTICE GUIDELINE Page 4
TOOLS FOR ASSESSING CORONARY ARTERY DISEASE Page 5
HISTORY Page 5
PHYSICAL EXAMINATION Page 7
ECG Page 7
ACUTE CORONARY SYNDROME Page 9
PATIENT SELECTION FOR ACCELERATED EVALUATION FOR ACS Page 13
DIAGNOSTIC STRATEGY FOR ACCELERATED EVALUATION Page 14
ECG Page 16
BIOCHEMICAL MARKERS Page 16
ETT Page 18
TREATMENT Page 20
SUMMARY & CONCLUSION Page 21
REFERENCES Page 22
LIST OF TABLES & FIGURES TABLE l:Key Diagnostic Items To Be Elicited for Assessing Significant CAD in Patients with Chest Pain Page 10
TABLE 2: Assessing the Likelihood of Significant CAD in Patients with Symptoms of Acute Coronary Syndrome Page 11
Risk Stratification Algorithm Page 14
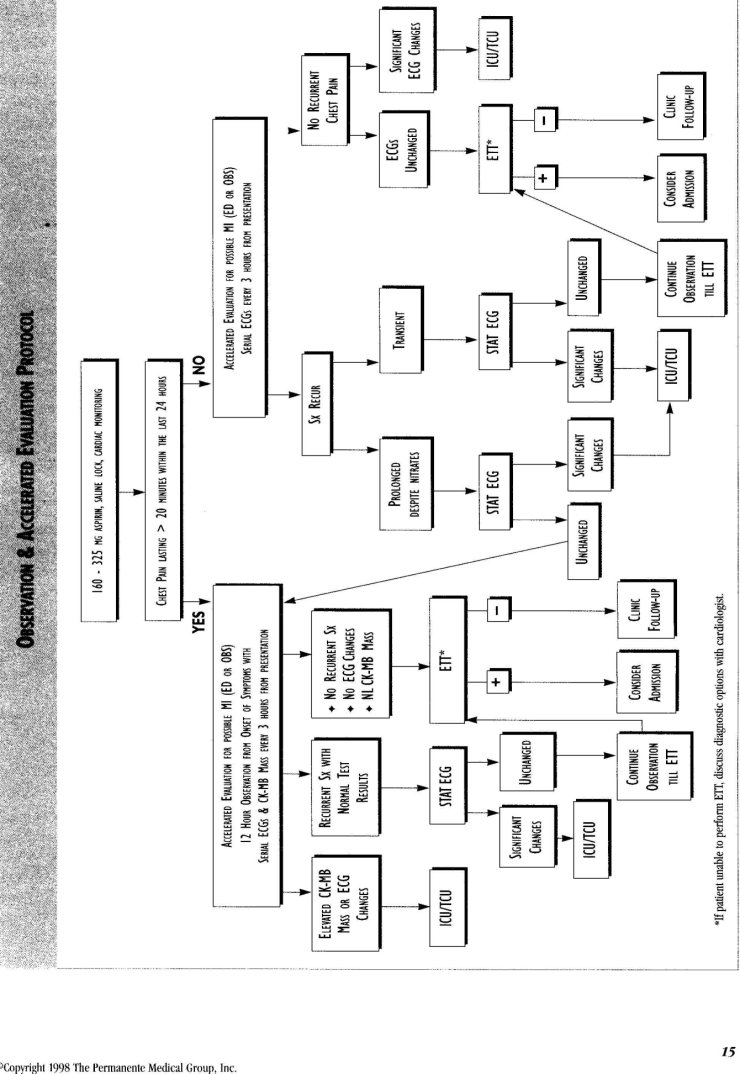
Observation & Acceleerated Evaluation Protocol Page 15
Standard tools for diagnosis are the clinical history, physical examination and ECG. New understanding of the pathophysiology of coronary artery disease has led to advances in treatment, particularly the use of thrombolytics and primary angioplasty.
Many medical centers have set the administration of thrombolytics within 30 minutes of patient arrival in the ED as a standard.
INTRODUCTION
BACKGROUND: CHALLENGES & SIGNIFICANCE OF CHEST PAIN EVALUATION
The evaluation of chest pain in the Emergency Department is a complex diagnostic problem. Standard tools for diagnosis are the clinical history, physical examination and ECG. However, these tools are imperfect for diagnosing acute coronary events that require hospitalization. The initial evaluation fails to readily diagnose almost 25% of acute myocardial infarction (AMI) patients.¹
Current medical practice is to maintain a low threshold for hospital admission to ensure that AMI or other acute coronary events are not missed. However, this has resulted in the admission of many patients to evaluate AMI who do not require hospitalization. Nationally, only about 30% of all admissions to the CCU actually have AMI and about 50-60% have acute ischemia² and not all of the latter group require hospitalization.³ From Sept 1996 until Sept 1997 at Northern California Kaiser Permanente, about 31% of all Emergency Department chest pain patients were admitted to the hospital; however, this varied from 17% to 42% among facilities. Of those admitted, only 18% had an AMI diagnosis at discharge (range across facilities was 11% to 31%) and another 24% had a diagnosis of unstable angina at discharge (range was 12% to 41%)[4] Other patients were admitted for evaluation because they had a suspicious clinical presentation and there were no existing alternative evaluation strategies in the Emergency Department. These practices have substantial implications for cost as well as quality of care. Nationally, it may cost as much as $13 billion dollars to care for these patients in the CCU[5].
New evidence and treatments suggest that a rapid and accurate strategy for identification of acute coronary events is necessary. New understanding of the pathophysiology of coronary artery disease has led to advances in treatment, particularly the use of thrombolytics and primary angioplasty. Greater pressure is being placed on practitioners to make rapid and accurate diagnoses since reperfusion of myocardium within the first two hours of an acute infarction can preserve ventricular functions and reduce mortality by nearly 50%[7] when compared with later reperfusion. Many medical centers have set the administration of thrombolytics within 30 minutes of patient arrival in the ED as a standard[8]. Public awareness of these new treatment modalities is high because of campaigns to increase awareness of the necessity for early diagnosis of AMI.
Such heightened public awareness may lead to two problems. First, as our members become more aware of the signs and symptoms of cardiac disease, patient groups with a lower prevalence of coronary artery disease (CAD) may seek evaluation for chest pain. Thus, while the number of patients presenting to EDs with chest pain may rise, the percentage who will eventually be diagnosed with an acute coronary syndrome may go down. As a corollary, the rates of false positives for diagnostic tests such as biochemical markers and exercise treadmill testing (ETT) may go up as the prevalence rate goes down in the tested population, leading to more unnecessary testing.
Secondly, patients with chest pain may arrive earlier after the onset of pain, a time when the initial diagnostic tools, particularly biochemical markers, are least reliable. We will need to have a strategy for evaluating patients quickly without giving them either cause for concern or an unnecessary cardiac diagnosis.
Finding the best setting for the evaluation of chest pain patients in terms of quality and cost has been a research issue since the 1980's. The possibility that CCUs were not required settings for the evaluation of uncomplicated chest pain patients was raised in the Multicenter Chest Pain Study[9]. A cost analysis using national data showed the CCU was nearly $300 million more expensive than stepdown units and the number of lives saved by this investment was 145 per year¹º.
More recently, attention has been turned to developing strategies for accelerated evaluation of patients with chest pain in short stay observation or clinical decision units, often placed in Emergency Departments. There has been proliferation of such units over the past decade with an estimated 1600 operating in 1995 and this trend continues to increase¹¹. The rationale for accelerated evaluation generally include improved diagnostic accuracy and risk management, improved patient satisfaction due to a shortened time frame to definitive diagnosis for the chest pain, more cost effective evaluation for the chest pain episode and an enhanced facility profile as a result of community outreach programs[12,13,14,15].
The goal of this guideline is to provide tools for the evaluation of patients with possible acute coronary syndrome after diagnoses of acute transmural myocardial infarction and noncardiac chest pain have been excluded.
GUIDELINE PROCESS
With these considerations in mind, a team of Internists, Cardiologists and Emergency physicians from the Northern California region met under sponsorship by TPMG Department of Quality and Utilization to develop a clinical practice guideline for the rapid evaluation of acute coronary events in the Emergency Department. The mandate of this group was to develop a clinical practice guideline which could help physicians risk stratify patients who present with non-traumatic chest pain and develop management strategies for those in whom there is continued uncertainty about the diagnosis of acute coronary syndrome.
In developing these guidelines, team members undertook an extensive literature search, spoke with several nationally recognized experts, and also considered data from Kaiser Permanente, Northern California Region.
This guideline was piloted at the San Francisco and South San Francisco Medical Centers from March to October of 1997. The pilot study was designed to evaluate all of the components of the guideline and allow definitive statements to be made about the efficacy of the suggested strategy. Unfortunately, the numbers of patients seen in the pilot were insufficient to allow an extensive analysis of efficacy. However, the pilot has provided an opportunity to examine the feasibility of operationalizing the guideline in two Emergency Departments as well as providing some data concerning the efficacy of some of the guideline components. This has been included in the text at the appropriate points. However, many of the guideline components have been validated in large clinical trials and appropriate reference to the literature is made. Comments and suggestions should be addressed to Christina Shih, MD at 415-202-4055.
CLASSIFICATION & GRADING OF RECOMMENDATIONS
Each guideline recommendation is justified in terms of the level of research evidence supporting it and the degree of consensus on it among the members of the work group. The distinction between support derived from scientific studies and that derived from expert opinion is important. Well-performed and relevant scientific studies provide a higher standard of evidence when they are available, but many aspects of medical care have not been addressed by such studies. Expert judgments supplement research evidence by factoring in clinical experience and human values that are not easily captured in scientific studies, and by extrapolating from scientific findings that were obtained with specific populations under specific conditions to a broad clinical context.
Support for recommendations is characterized as follows:
GRADE A Supported by the results of two or more randomized clinical trials (RCTs) that have good internal validity, and also specifically address the question of interest in a group of patients comparable to the one to which the recommendation applies (external validity).
* The goal of this guideline is to provide tools for the evaluation of patients with possible acute coronary syndrome after diagnoses of acute transmural myocardial infarction and noncardiac chest pain have been excluded.*
GRADE B
Supported by a single RCT meeting the criteria given above for "Grade A"-level evidence; by RCTs that only indirectly address the question of interest; or by two or more non-randomized clinical trials (case control or cohort studies) in which the experimental and control groups are demonstrably similar or multivariate analyses have effectively controlled for group differences.
GRADE C
Supported by a single non-RCT meeting the criteria given above for "Grade B"-level evidence, by studies using historical controls, or by studies using quasi-experimental designs such as pre- and post-treatment comparisons.
EXPERT OPINION: STRONG CONSENSUS
Agreement among at least 90% of the guideline work group members and expert reviewers.
CONSENSUS
Agreement among at least 75% of the guideline work group members and expert reviewers.
Classifications adopted from U.S. Dept. of Public Health, Agency for Health Care Policy and Research.
OVERVIEW of CLINICAL PRACTICE GUIDELINE
This guideline is intended to provide tools for physicians who must decide whether the chest pain is due to an acute coronary syndrome and, if so, whether the syndrome is of sufficient severity to warrant hospital admission. All of our Emergency Departments have a priority triage system that allows chest pain patients to be evaluated immediately. It is recommended that a 12 lead ECG be obtained in less than five minutes of the patient's arrival, and that the physician begin immediate evaluation.
The first step in the guideline is the use of the clinical interview, physical examination and 12- lead electrocardiogram (ECG) to assess the likelihood of significant CAD (Table2). The guideline begins with the physician first determining if the etiology of the chest pain is acute myocardial infarction, possible angina or MI, or noncardiac. For management of patients with recognized acute transmural myocardial one should refer to Clinical Practice Guidelines for the Treatment of Acute Myocardial Infarction published by TPMG[8]. Patients having non-cardiac chest pain are outside the scope of this chest pain guideline and should have the appropriate evaluation and treatment. The focus of this guideline applies to patients whose initial diagnostics are indeterminate and for whom there is still concern over the possibility of acute coronary syndrome.
Patients are then assessed for their short term risk of immediate complications or death: high, intermediate or low. Those with a high risk of complications are admitted to the ICU/TCU and those with a low risk are referred for an outpatient evaluation. Outpatient evaluation should occur within 72 hours and should include stress testing when appropriate. The results of testing should be transmitted to the primary care physician along with notification from the ED that the patient was seen in the ED.
Patients with an intermediate risk of complications require further diagnostic evaluation conducted either in the Emergency Department or another area of the hospital. This guideline primarily addresses the selection, diagnostic strategies and disposition of patients with intermediate risk of complications.
GUIDELINE GOALS
* To assist practitioners in distinguishing among patients with acute coronary syndromes (AMI, unstable angina), stable angina and noncardiac chest pain
* To assist practitioners in accurately stratifying patients with possible acute coronary syndrome into high, moderate or low risk of morbidity or mortality
* To minimize the number of patients discharged from the ED with unrecognized myocardial infarction or unstable angina
* To decrease the hospitalization rates for patients having noncardiac chest pain. The accelerated evaluation will result in earlier diagnosis and decreased hospital length of stay. These two features will decompress our often crowded critical care areas and improve overall hospital efficiencies
* To increase patient satisfaction by providing earlier and more definitive diagnosis of either cardiac or noncardiac causes for their chest pain symptoms
* To increase physician satisfaction by providing a strategy that minimizes the uncertainty of the ultimate diagnosis upon discharge from the ED without over utilizing resources or jeopardizing patient safety
TOOLS' ASSESSING CAD
THE HISTORY: THE MOST IMPORTANT DIAGNOSTIC TOOL
Despite a vast and growing array of ancillary diagnostic strategies including biochemical markers, exercise treadmill testing, nuclear imaging studies, and continuous 12 lead ST segment monitoring, the most important diagnostic tool to determine the need and scope for further workup continues to be the patient history taken by a skillful and experienced clinician. Key diagnostic items to be elicited for assessing chest pain include (for a brief synopsis refer to Table 1): * time of onset of pain * duration of pain * characterization of the pain including radiation to neck, jaw, back, shoulders or arm * associated symptoms, such as shortness of breath, diaphoresis or nausea * previous history of AMI or invasive procedures such as coronary artery bypass grafting (CABG) or angioplasty (PTCA) * other risk factors for CAD, such as hypercholesterolemia, hypertension, diabetes or family history * illicit drug use
Time of onset of chest pain is critical for determining whether the patient should receive thrombolytic agents if an AMI is present. Additionally, the sensitivity and specificity of many biochemical markers used to diagnose non-Q-wave infarctions are dependent upon the length of time from onset of symptoms.
The diagnosis of unstable angina is also time dependent. Some classification systems include any new onset angina as unstable angina; however, others consider it too inclusive a definition (since even stable angina has a first episode and the new onset) which will result in inappropriate admission of many patients with new chest pain but not unstable angina.
*Time of oneset of chest pain is critical for determining whether the patient should receive thrombolytic agents if an AMI is present. *Additionally, the sensitivity and specificity of many biochemical markers used to diagnose non-Q-wave infarctions are dependent upon the length of time from onset of symptoms.*
*The management of patients over age 65 continues to be more complex and demanding than of younger patients. *Diabetes, cigarette smoking, hypercholesterolemia, and hypertension are important predictors of significan CAD. *Althought women have a 50% lower risk of AMI than men after adjustment for age, care must be taken since it has been shown that women with chest pain are less aggressively evaluated.
Knowing the duration and persistence of pain is very helpful in the classification of chest pain. Features suggestive of noncardiac chest pain include constant pain lasting days or fleeting pain lasting a few seconds or less. One study found that patients who had chest pain that was either persistent upon arrival or recurred during the ED evaluation had a 2.3 times greater risk of requiring interventions (such as IV lidocaine or nitroglycerine temporary pacing, pressor support, cardioversion, angioplasty, CABG, thrombolytics or ventilator support), a 1.7 times greater risk of complications (minor dysrhythmias, pump failure, recurrent chest pain), a 3.8 times greater risk of life-threatening complications (severe dysrhythmias), and 2.4 times greater risk of having an AMI than patients whose pain had resolved prior to arrival in the ED[16].
Knowledge of the character of the pain is somewhat helpful. Pain which is pleuritic, reproduced by movement or palpation of the chest or arms, or localized with one finger is suggestive of noncardiac chest pain but does not completely exclude the diagnosis of ischemic pain. In the large Multicenter Chest Pain Study, 23% of patients complaining of "burning or indigestion" pain had an MI and 21% had unstable angina. In those complaining of a "knot, suffocating, bricks, or indescribable" chest pain, 23% had an MI. Of patients with "sharp or stabbing" pain, 5% had an MI and 17% unstable angina[17].
Associated symptoms which are helpful in assigning a cardiac diagnosis include shortness of breath, nausea, sweatiness, or lightheadedness[18]. These symptoms, like chest discomfort, may be exertional or occur at rest. They are not generally useful in isolation, with the possible exception of shortness of breath.
Likelihood factors for coronary artery disease are used in the Agency for Health Care Policy and Research (AHCPR) guideline for Unstable Angina[3] to assess the likelihood of significant coronary artery disease in patients with symptoms suggestive of acute coronary syndrome.
History of prior AMI or significant invasive procedures. Prior myocardial infarction as determined by history or ECG findings of Q waves or a history of invasive procedures for CAD such as CABG or PTCA are the most important indicators of severe CAD.
Age. Among elderly patients (over age 65), the relative importance of clinical features such as male gender, pressure-like quality of pain, radiation of pain and ECG changes are diminished and therefore less helpful. Studies have shown that the elderly are more often admitted to intensive care units, yet rule in for AMI less frequently than younger patients with the same ECG findings. Older patients are also less likely to have typical symptoms when they do rule in for AMI. Thus, elderly patients with severe CAD may be less likely to be admitted because of the atypicality of their symptoms. Paradoxically more elderly patients without CAD are unnecessarily admitted to intensive care units. The management of patients over age 65 continues to be more complex and demanding than of younger patients[19].
Number of associated risk factors such as diabetes, smoking, hypertension, and hypercholesterolemia.
Diabetes is the most important risk factor carrying twice as much weight as two or more other risk factors[3], but cigarette smoking, hypercholesterolemia, and hypertension are also important predictors of significant CAD. In addition, it has been shown that diabetics have a higher prevalence of previously diagnosed cardiovascular disease[20].
Gender. Although women have a 50% lower risk of AMI than men after adjustment for age, care must be taken since it has been shown that women with chest pain are less aggressively evaluated, with more time elapsing between the time of physician evaluation and the obtaining of an ECG [21]. When found to have an AMI, women were not as likely to be admitted to ICUs when compared with men (56% vs. 83%)[22].
Drug Use. Cocaine and amphetamine abuse can cause both MIs and unstable angina. A careful history should be taken regarding the possibility of drug abuse in younger patients presenting with chest pain since the prevalence of cocaine use has been found to be surprisingly high in a suburban/urban group of patients evaluated for chest pain in Detroit (29% in the 18-30 year old group; 48% in the 31-40 year old group; 18% in the 41-50 year old group and 3% in the 51-60 year old group) [23]. Although these prevalence statistics have not been confirmed in other metropolitan areas, consideration should also be given to using drug tests to detect use since patient history is frequently unreliable. Caution should be exercised in interpreting abnormal biochemical marker results in these patients because cocaine can cause an elevation of serum CK enzymes that are unrelated to AMI[24].
RECOMMENDATION A complete history with defined elements including characterization of the discomfort, associated symptoms and risk factors is the crucial starting point for evaluation of patients with possible acute coronary syndrome (Strength of evidence =B ).
PHYSICAL EXAMINATION
Physical findings suggestive of ischemic disease include the presence of an S4, S3 or new mitral insufficiency murmur. The presence of rales above the bases has prognostic significance. In addition, signs of causes of secondary unstable angina should be sought such as: * Pallor and tachycardia from anemia * Pulse abnormalities suggesting dysrhythmias such as atrial fibrillation, bradycardias * Proptosis, thyromegaly, hyperactive reflexes, tachycardia, skin changes to suggest hyperthyroidism
It is beyond the scope of this clinical guideline to address other cardiovascular causes of chest pain such as aortic dissections and pericarditis, but these should be kept in mind by the clinician. Similarly, the myriad noncardiac causes of chest pain and diseases such as pleuritis, pulmonary embolism, pneumonia, or pneumothorax should be sought during the physical exam.
RECOMMENDATION Careful performance and documentation of physical examination is essential to appropriate evaluation of chest pain patients. Important findings include the presence of an S4, S3 or new mitral insufficiency murmur, rales above the bases, pallor and tachycardia, pulse abnormalities, proptosis, thyromegaly, or hyperactive reflexes (Strength of evidence =B).
THE ECG THE ROLE OF THE ECG 12-lead ECGs should be obtained as quickly as possible when patients present with chest pain as stated in departmental policy and procedures or standing orders without waiting for a physician to order the ECG. ED personnel should show the ECGs to a physician for interpretation as soon as possible. Significant ST elevations not known to be old that persist despite nitrates indicate that the patient is having an acute MI and should be referred to the Kaiser Permanente AMI guidelines[8].
ECG interpretation skills on the part of the examining physician are crucial for accurate diagnosis. In a study of patients discharged from the ED and subsequently found to have MI, 25% were found to have had ECG abnormalities present on the ED ECG that were missed by the examining physician[25]. It is strongly encouraged not to rely on computer generated ECG interpretations as they may be misleading.
Although history is the major determinant of risk stratification, certain ECG findings are important in determining the disposition of the patient to an intensive care unit, lower level step-down unit, short-stay unit, or home with an outpatient evaluation.
*12-lead ECGs should be obtained as quickly as possible when patients present with chest pain as stated in departmental policy and procedures or standing orders without waiting for a physician to order the ECG. *It is strongly encouraged not to rely on computer generated ECG interpretations as they may be misleading.
*Numerous studies have shown that a normal ECG or one having minimal nonspecific abnormalities does not exclude an AMI. *If one suspects an AMI with new LBBB, thrombolysis should be considered according to the Kaiser Permanente AMI guideline. *Although history is the major determinant of risk stratification, certain ECG findings are important in determining the disposition of the patient to an intensive care unit, lower level step-down unit, short-stay unit, or home with an outpatient evaluation.
IMPORTANT ECG CHANGES IN ASSESSING THE PROBABILITY OF SIGNIFICANT CAD According to the AHCPR guidelines, patients have a high likelihood of significant CAD if the ECG shows: * ST increase or decrease ³1 mm * Marked symmetrical T wave inversions in multiple precordial leads * Dynamic changes with chest pain
There is an intermediate likelihood of CAD if the ECG shows: * ST depression .5 to I mm * T wave inversion ³ 1 mm in leads with dominant R waves
There is a low likelihood of CAD if the ECG shows: * A normal ECG * T wave flat or inverted < 1 mm in leads with dominant R waves
ST depressions and deeply inverted T waves not known to be old, place the patient in a high risk category and the patient should be admitted. Patients with unstable angina and an abnormal ECG have 2.9 times the risk of needing interventions in the near future and 14.2 times the risk for an AMI compared with those patients who have a normal ECG[26].
Patients with chest pain having new left bundle branch block (LBBB) are at high risk for having CAD and should probably be admitted depending on the acuity of the history. If one suspects an AMI with new LBBB, thrombolysis should be considered according to the Kaiser Permanente AMI guideline[8].
Left ventricular hypertrophy can cause secondary T wave inversions and ST changes which can be indistinguishable from those caused by ischemia. Old ECGs for comparison are critical in interpreting these ECGs correctly.
VASOSPASTIC ANGINA Dynamic changes with chest pain ST elevations that are transient and are relieved with nitrates occurring in a younger patient with few cardiac risk factors should suggest vasospastic angina. However, since it is impossible to differentiate vasospastic angina with its more benign prognosis from more typical angina without cardiac catheterization, these patients should be admitted for evaluation by a cardiologist
SIGNIFICANCE OF A NORMAL ECG Numerous studies have shown that a normal ECG or one having minimal nonspecific abnormalities does not exclude an AMI. In one study, three percent of patients with AMI had an initially normal ECG and seven percent had only nonspecific ST changes. These patients tended to be male, over 50 years old, and to have typical chest pressure with radiation. They were less likely to have diaphoresis or a previous history of ischemic heart disease[27]. In another study, 10% of patients with normal ECGs and 8% of those with nonspecific ECG changes were found to have an AMI[28].
However, these and other studies[29] have shown that those patients with normal or minimally abnormal ECGs with an AMI have later peaking and lower levels of cardiac enzyme elevations. Additionally, despite having an AMI or unstable angina, patients with a normal or nonspecific ECG on admission are at lower risk for complications and death.
RECOMMENDATION The initial assessment of patients with a 12-lead ECG in the ED is at the center of the decision pathway because of the strong evidence that ST-segment elevation identifies people who benefit from reperfusion therapy. Many patients with a normal or with nonspecific ST changes can be safely evaluated in either short stay or step down units rather than in intensive care units (Strength of evidence = B).
ECG READING SKILLS ARE IMPORTANT
In the Multicenter Chest Pain Study[9] ( N=3077) 4% of patients with MIs were sent home from the ED. Of these patients, only 31% were captured by their return to the ED for persistent symptoms. The other 69% were only detected by the follow-up procedures of the study. On reviewing the ED visit of all these patients with missed MI, 49% would have been correctly identified with better ECG interpretation skills or by appropriate admission of patients with ischemic symptoms. In approximately 25% of patients with missed MIs, the physician made an incorrect management decision (discharge home) despite having made the correct diagnosis of ischemic disease by history. In general, these patients were younger, had less typical symptoms, were less likely to have angina or an MI in the past, or to have new ECG changes. In another multicenter study[30], 1.9% of patients with AMI were discharged from the ED (from a total of 1,050 patients). Of these patients, 25% had ST elevation and 35% were diagnosed with ischemic heart disease but were still discharged. Death or potentially lethal complications occurred in 25% of these missed MI patients. Again, the authors concluded that better ECG reading skills and admission of patients recognized to have ischemic heart disease would have prevented these inappropriate discharges.
COMPARISON WITH OLDER ECGs
Another issue of importance is the availability of old ECGs for comparison. It has been shown that the availability of a prior ECG led to more appropriate discharges home or admissions to lower acuity hospital beds when ECG changes were known to be old[31]. We recommend that previous ECGs be readily available to providers. This can be accomplished by fax transmission of ECGs from ECG departments or medical records, computerized storage and retrieval systems, better availability of medical records to providers and giving patients copies of their ECGs to bring with them.
RECOMMENDATION Excellent ECG interpretation skills by clinicians need to be encouraged with careful attention to ST segments. The availability of prior ECGs is crucial for interpretation of ECG abnormalities and mechanisms should be instituted to ensure rapid access to prior ECGs at all times (Strength of evidence = C).
ACUTE CORONARY SYNDROME
Acute coronary syndrome (ACS) refers to the acute presentation of patients having CAD. It includes a spectrum of illness ranging from the first onset of angina up to and including acute myocardial infarction (subendocardial and transmural). It excludes patients with chronic stable angina. The problem the clinician faces while evaluating these patients lies in determining the risk of death or serious morbidity along this spectrum. More accurate determination of risk has been shown to result in better selection of the most appropriate level of care (ICU admission, TCU admission, observation and evaluation in the ED, discharge home) [32].
Assessing the likelihood of CAD is the first step in determining the prognosis of a patient who presents with symptoms that suggest acute coronary syndrome. Table 2 summarizes the important factors to consider when making this decision.
*Another issue of importance is the availability of old ECG's for comparison. It has been shown that the availability of a prior ECG led to more appropriate discharges home or admissions to lower acuity hospital beds when ECG changes were known to be old. *Acute coronary syndrome (ACS) refers to the actute presentation of patients having CAD. It includes a spectrum of illness ranging from the first onset of angina up to and including acute myocardial infarction (subendocardial and transmural).
Table 1:Key Diagnostic Items to be Elicited for Assessing Significant CAD in Patients with Chest Pain Suggestive of Acute Coronary Syndrome ITEM RATIONALE Time of Onset of Pain *Critical for determining whether the patient should receive thrombolytic agents if an AMI is present *Sensitivity and specificity of cardiac markers are time dependent Duration and Persistence of pain Helpful in the classification of chest pain. Features suggestive of noncardiac chest pain include constant pain lasting days or fleeting pain lasting a few seconds or less Character of Pain Pain which is pleuritic, reproduced by movement or palpation of the chest or arms, or localized with one finger is suggestive of noncardiac chest pain but does not completely exclude the diagnosis of ischemic pain. Associated symptoms Helpful in assigning a cardiac diagnosis, they include shortness of breath, nausea, sweatiness, lightheadedness History of prior AMI or significant invasive procedures Prior AMI as determined by history or ECG findings of Q waves or a history of invasive procedures for CAD such as CABG or PTCA are the most important indicators of severe CAD Age and Gender Older age and male gender have been consistently shown to be predictive of MI or USA in the ED setting. The management of patients over age 65 continues to be more complex and demanding than of younger patients. It has also been shown that women with chest pain are less aggressively evaluated Number of associated risk factors Diabetes is the most important risk factor, but cigarette smoking, hypercholesterolemia, and hypertension are also important predictors of significant CAD Drug Use *Cocaine and amphetamine abuse can cause both Mis and unstable angina *Cocaine can also cause an elevation of serum CK enzymes that are unrelated to AMI Physical Exam *Physical findings suggestive of ischemic disease include the presence of an S4, S3 or new mitral insufficiency murmur. The presence of rales above the bases has prognostic significance *In addition, signs of causes of secondary unstable angina should be sought such as:pallor and tachycardia from anemia; pulse abnormalities suggesting dysrhythmias such as atrial fibrillation, bradycardias; proptosis, thyromegaly, hyperactive reflexes, tachycardia,skin changes to suggest hyperthyroidism ECG *High likelihood of CAD if: ST increase or decrease ³ 1 mm; Marked symmetrical T wave inversions in multiple precordial leads; dynamic changes with chest pain * Intermediate likelihood of CAD if: ST depression .5 to 1 mm; T wave inversion ³ 1 mm in leads with dominant R waves * Low likelihood of CAD: A normal ECG; T wave flat or inverted < 1 mm in leads with dominant R wavesANGINA
STABLE ANGINA
Stable angina is believed to be caused by fixed atheromatous lesions and typically is clearly related to exertion or stress and relieved by rest or nitrates. Patients usually complain of substemal chest or arm pain or pressure which is poorly localized. Anginal equivalents should be considered when patients complain of jaw, neck, ear or arm discomfort or dyspnea with exertion or stress. Obviously every patient having stable angina has a first episode and it is difficult to predict the severity of CAD at the time of first onset. Clearly not every patient with new angina needs admission to an ICU and this guideline is intended to help practitioners with evaluation strategies to detect patients with more severe disease. TABLE 2: ASSESSING THE LIKELIHOOD OF SIGNIFICANT CAD IN PATIENTS WITH SYMPTOMS OF ACUTE CORONARY SYNDROME HIGH LIKELIHOOD INTERMEDIATE LIKELIHOOD LOW LIKELIHOOD Any of the following features: No high likelihood features and any of the following: No high or intermediate likelihood and any of the following: History prior MI or other CAD Definite angina: males >60 or females>70 years of age Non-Anginal Chest Pain Definite angina: males >60 or females >70 years of age Probable angina: males³ 60 or females ³70 years of age One risk factor other than diabetes Transient hemodynamic or ECG; changes during pain Chest pain probably not angina in diabetics T-wave flattening or inversion <lmm in leads with dominant R-waves Variant Angina (pain with reversible ST-segment elevation) Chest pain probably not angina and 2-3 risk factors* other than diabetes Normal ECG ST segment-elevation or depression ³lmm Extracardiac vascular disease Maraked symmetrical T-wave inversion in multiple precordial leads ST depression .5 to 1mm T-wave inversion ³1mm in leads with dominant R-waves *CAD risk factors are diabetes, smoking hypertension and elevated cholesterol.Reproduced from: AHCPR, Unstable Angina; Diagnosis and Management, 1994 Note: Estimation of the likelihood of significant CAD is a complex, multivariate problem that cannot be fully specified in a table. This is not a ripid algorithm but rather suggests important considerations.
*Stable angina is believed to be caused by fixed atheromatous lesions and typically is clearly related to exertion or stress and relieved by rest or nitrates.
*TIMI IIIB trial has shown that thrombolytics are not useful in non-Q wave infarctions or unstable angina; however, the use of aspirin, heparin, nitrates, beta blockers, nangioplasty and coronary bypass surgery may be indicated in a subset of patients with unstable angina who are at the high risk for death*
UNSTABLE ANGINA,
According to the AHCPR guideline3, unstable angina is defined as a clinical syndrome that falls between stable angina and acute MI in the spectrum of coronary artery disease and has three possible presentations: prolonged angina at rest (> 20 minutes); new onset (< 2 months) of exertional angina of at least Canadian Cardiovascular Society Classification (CCSC) Class III in severity, or recent (< 2 months) acceleration of angina to at least CCSC Class III. Anginal equivalents, non-Q-wave MI and post-MI (>24 hours) angina are part of the spectrum of unstable angina.
Primary unstable angina is now believed to be caused by rupture of an atheromatous plaque, subsequent thrombus formation and partial occlusion of a coronary vessel. Secondary unstable angina can occur in patients who have previously stable angina but develop destabilizing conditions such as anemia, hypoxemia, dysrhythmias, fever, hyperthyroidism, environmental or emotional stress.
Although a significant percentage of patients with unstable angina may progress to a complete infarction, there is a wide spectrum of risk for complications and death. There is similarly a wide spectrum of treatment options. TIMI IIIB trial has shown that thrombolytics are not useful in non-Q wave infarctions or unstable angina; however, the use of aspirin, heparin, nitrates, beta blockers, angioplasty and coronary bypass surgery may be indicated in a subset of patients with unstable angina who are at high risk for deaths. These patients should be managed in step-down or intensive care units. At the other end of the spectrum, it has been estimated that as many as 50% of patients with unstable angina are at low risk for death and therefore do not require admission to an intensive care or coronary care unit. The CCSC* System to Categorize the Severity of Angina Description of State of Angina Class I Ordinary physical activity does not cause angina, such as walking, climbing stairs. Angina occurs with strenuous, rapid, or prolonged exertion at work or recreation Class II Slight limitation of ordinary activity. Angina occurs on walking or climbing stairs rapidly, walking uphill, walking or stair climbing after meals, or in cold, or in wind, or under emotional stress, or only during the few hours after awakening. Walking more than two blocks on the level and climbing more than one flight of ordinary stairs at a normal pace and in normal condition. Class III Marked limitations of ordinary physical activity. Angina occurs on walking one to two blocks on the level and climbing one flight of stairs in normal conditions and at a normal pace. Class IV Inability to carry on any physical activity without discomfort. Anginal symptoms may be present at rest.*Canadiann Cardiovascular Society Classification System Source: Campeau L Grading of angina pectoris (letter). Circulation. 54:522-523,1976. Copyright 1976, American Heart Association, Inc. Used with permission.
PATIENT SELECTION for ACCELERATED EVALUATION for ACUTE CORONARY SYNDROME
The most critical element for successful outcomes (no missed MIs, no inappropriate discharges, no adverse results from early exercise testing, no delays in treatment) is the accurate estimation of risk and appropriate patient selection for the various treatment arms in the algorithm which follow. It is vital that physicians read and fully understand the criteria for estimation of risk and understand the rationale that underlies the use of the accelerated evaluation protocol.
A multicenter study involving thousands of patients[32] showed that two major sets of factors predict subsequent development of major cardiac events (defined as ventricular fibrillation, cardiac arrest, new complete heart block, insertion of a temporary pacemaker, emergency cardioversion, cardiogenic shock, use of an intra-aortic balloon pump, intubation, or recurrent ischemic chest pain requiring CABG or PTCA) over the next 72 hours and thus require admission to an ICU. The first set of factors could be determined on initial presentation and include male sex, older age, pain described as the same as during a prior MI or worse than usual angina, systolic blood pressure below 100 mm Hg, rales above the bases and ECG changes suggestive of acute myocardial infarction or ischemia. In a subsequent analysis after adjusting for the patient's characteristics at initial presentation the following set of factors were stronger predictors of development of major cardiac events within 72 hours. These include the development of major or intermediate events (defined as atrial flutter, AV dissociation, Mobitz I or II block not treated with a pacemaker, sinus bradycardia treated with medications, pulmonary edema without hypotension, recurrent ischemic pain not requiring CABG or PTCA) or documented MI during the first 12 hours of observation. The study also reported that appropriately selected patients (based on initial ECG, physical exam and historical findings) who did not develop an intermediate or major cardiac event during a period of 12 hours of observation were not likely to develop any major cardiac event beyond the 12 hour period of observation.With information from this and other studies, the following strategy is recommended:
*Based on the initial history, physical exam and ECG, all patients with acute transmural MIs should be treated in accordance to the AMI guideline[8]. All patients thought to have noncardiac chest pain should exit this guideline.
*The next step is assessing the short term risk of death or MI (refer to algorithm on page 14). Any patient who has previously had an MI or invasive cardiac procedure (CABG or PTGA) who complains of similar chest pain or any patient with documented angina who complains of chest pain worse than their usual should be admitted. Any patient having high risk features listed in the algorithm should be admitted.
*Patients with no high risk features and at least one intermediate risk feature should be managed according to the accelerated evaluation protocol (refer to algorithm on page 15). Patients who have had one or more episodes of sustained chest pain lasting more than 20 minutes within the 24 hours prior to presentation should have serial CK-MB mass determinations and ECGs as detailed in the left hand portion of the algorithm. Patients without sustained chest pain lasting more than twenty minutes are unlikely to have had an infarction. Therefore in general they do not need biochemical marker testing. These patients should be observed as detailed in the right hand portion of the algorithm until treadmill testing can be accomplished. If a patient awaiting treadmill develops significant chest pain with dynamic ECG changes they should be admitted for unstable angina. If there is chest pain longer than 20 minutes and no ECG changes then the patient should be evaluated with serial CK-MB mass determinations and ECGs.
*Patients at low risk, as defined by the algorithm, may be discharged with follow up and if appropriate an Exercise Treadmill Testing (ETT) scheduled within 72 hours.
*The most critical element for successfitl outcomes (no missed MIs, no inappropriate discharges, no adverse results from early exercise testing, no delays in treatment) is the accurate estimation of risk and appropriate patient selection for the various treatment arms in the algorithm • A multicenter study reported that appropriately selected patients (based on initial ECG, physical exam and historical findings) who did not develop an intermediate or major cardiac event during a period of 12 hours of observation were not likely to develop any major cardiac event beyond the 12 hour period of observation.
 *Once patients enter
the accelerated evaluation protocol,
they should have 12-lead ECG's at least
every 3 hours.
*Once patients enter
the accelerated evaluation protocol,
they should have 12-lead ECG's at least
every 3 hours.
*Current data n the literature and the clinical experience obtained in the chest pain pilot study do not support use of continuous ST-segment monitoring.
*Multiple investigations have shown that a single, isolated measurement of serum CK is insensitive and nonspecific for acute infarction in the initial setting.
THE ECG
Once patients enter the accelerated evaluation protocol, they should have 12-lead ECGs at least every 3 hours. Current data in the literature and the clinical experience obtained in the chest pain pilot study do not support use of continuous ST-segment monitoring[34].
BIOCHEMICAL MARKERS
ROLE OF BIOCHEMICAL MARKERS As previously mentioned, numerous studies[2,14] have shown that up to 70% of patients admitted to the CCU for possible AMI have not had an AMI. The patient's history and ECG are the most important factors in the evaluation of chest pain in the ED while biochemical markers or "cardiac enzymes" are useful in determining the need for ICU/TCU admission in selected patients with prolonged chest pain and nondiagnostic ECGs.
Myocyte necrosis is associated with the loss of cell membrane integrity and diffusion of macromolecules into the interstitium. These proteins then appear in the intravascular space. Their pattern of appearance in the blood depends on molecular weight, local blood flow and clearance from the system. A variety of these markers can be measured in the laboratory including creatinine kinase and its isoenzymes and their subforms, LDH, myoglobin and troponins. These markers have characteristic patterns of release following myocardial infarction[35].The dynamic sequence of events that occurs during AMI is central to the rationale of sequential measurement of various biochemical markers of infarction. As the appearance of markers in the circulation during myocyte injury is time dependent, measurement of biochemical markers over a given period of time provides improved sensitivity and specificity for detection of that injury. Multiple investigations have shown that a single, isolated measurement of serum CK is insensitive and nonspecific for acute infarction in the initial setting[36,37,38,39,40,41].
CREATINE KINASE CK-MB mass determination has been shown to have superior sensitivity and specificity over CK-MB activity and total CK. There is a large body of scientific evidence describing its applicability to the evaluation of patients with chest pain and nondiagnostic ECGs in the ED. The sensitivity is low in the first hours after the onset of chest pain but increases to >90% sensitivity within 9 hours of pain onset[42].
MYOGLOBIN Serum myoglobin (SMgb) is a relatively new biochemical marker that is gaining acceptance as a useful tool in the evaluation of possible AMI. It rises to abnormal levels as early as one to three hours after the onset of infarction and peaks two to five hours earlier than CK. The kidneys rapidly clear myoglobin from the circulation with elevated SMgb levels returning to normal within 12-24 hours [43, 44]. This may lead to false negative results in clinical use. SMgb also lacks tissue specificity and may be abnormally elevated in conditions such as skeletal muscle trauma, muscular dystrophy, vigorous exercise, myocarditis, cardiac surgery, shock and renal failure. SMgb may produce false positive tests for AMI if used in these conditions.
TROPONIN Cardiac troponins T and I are regulatory proteins found in the contractile apparatus of cardiac muscle and have been investigated as markers for AMI. During cell injury, troponins are released and appear in the circulation. Troponin levels may become abnormal as soon as 3 hours from myocardial injury and remain elevated for five days. The pattern of appearance of troponins in the serum and their clinical sensitivity in diagnosing MI at time intervals of up to 12 hours are similar to CK-MB mass.
Troponins are specific for myocardial injury but not specific for AMI. Slightly elevated troponin levels can be observed in the presence of myocardial ischemia without infarction.[45] Furthermore, elevated troponin levels are powerful, independent predictors of death and serious complications in patients with unstable angina.[46,47]REVIEW & EVALUATION OF BIOCHEMICAL MARKER LITERATURE
The Chest Pain Clinical Practice Guideline team reviewed more than 50 papers on biochemical markers for AMI. From this literature, we distilled a strategy for using biochemical markers in patients with chest pain suspected to have unstable angina and/or AMI. This discussion does not apply to the confirmation of acute AMI in patients with ECG changes characteristic of AMI or the unstable angina patient with high risk features as defined in this clinical practice guideline.
Sensitivity and specificity were chosen as the appropriate measures to compare data from different studies. Positive and negative predictive value depend upon the incidence of MI in the study population. The incidence of MI varies widely between studies because patients were selected by different criteria.The interpretation of a biochemical marker test depends on the time interval between the onset of symptoms and specimen collection. None of the biochemical marker tests has adequate sensitivity at the onset of symptoms. Each marker reaches a peak sensitivity at some time interval and then sensitivity declines. In physiologic terms, the interval from the onset of symptoms until specimen collection is the most important determinant of the sensitivity of a biochemical marker. However, in clinical practice the determination of symptom onset can be imprecise and subject to interpretation. If the patient history does not lend itself to documentation of an exact time of symptom onset it would be prudent to use the time interval from presentation to the ED to minimize ambiguity about the timing of blood samples for biochemical marker testing.
The guideline group set 90-95% sensitivity as the minimum acceptable sensitivity for any testing strategy. We then identified tests that met the threshold of sensitivity, the time interval in which a test met the threshold and the specificity of the test.
CK-MB mass was determined to be the most reliably sensitive biochemical marker. In all studies that measured CK MB at time intervals of six hours or greater from the onset of symptoms, our threshold of sensitivity was reached. Nearly all studies included CK-MB as one of the markers. Several studies included various combinations of total CK, CK-MB activity and CK-MB mass. In general, CK-MB mass is more sensitive, more specific or both than CK-MB activity or total CK. There were individual studies in which other biochemical markers met our threshold sensitivity and outperformed CK-MB but no test outperformed CK-MB mass in more than one study.CK isoforms have attracted some interest in the literature[48], however, a survey of Kaiser Permanente facilities nationwide shows little use of the isoforms, primarily because of the technical complexities of https://kaiserpapers.com/downey/cajue/evalcoro/ performing the test.
Myoglobin shows promise as a marker that may reach the desired sensitivity in a shorter interval than CK-MB mass. One study found myoglobin to be 100% sensitive as quickly as three hours after arrival in the ED; however, subsequent studies have not confirmed this.[49] Experience with myoglobin in the chest pain pilot project at SF and SSF Kaiser Medical Centers showed little clinical usefulness, a finding echoed in a recent survey of myoglobin use across Kaiser Permanente facilities nationwide[50]. It is the opinion of the guideline group that currently myoglobin measurement has no role in the evaluation for possible AMI.
Troponins are relatively new biochemical markers that show much promise in the diagnosis of MI. As discussed earlier, the sensitivity of troponins for diagnosing MI appears to be comparable to CK-MB mass. Troponins may also provide prognostic information for patients with unstable angina [51,52]. Several experts in the field have indicated that they believe troponins will replace CK-MB as the "gold standard" biochemical marker of MI in the near future and it is already being used at many large medical centers including the University of California at San Francisco.[53] During and after the pilot study conducted at SF and SSF, troponin I testing was performed using materials provided by three different vendors. It was determined that the results provided by different vendors testing the same blood samples were inconsistent. One vendor had a higher frequency of false negative results which was felt to pose a greater danger in clinical practice since these patients might be sent for early ETT or discharged inappropriately. Also, use of the normal, indeterminate and abnormal values provided by the vendors resulted in excessive numbers of false positive test results. At Santa Clara Kaiser, slightly higher cutoff values had to be established to avoid potential false-positive results and unnecessary hospitalization. Although we agree that the potential benefits of the use of troponin are intriguing, the difficulties we encountered in actual clinical use make further study necessary before we recommend widespread adoption of troponins throughout the region. The regional laboratory groups will need to first resolve the problems of intervendor variability and select the most reliable vendor and secondly establish normal/abnormal values for our patient population.
*In physiologic terms, the interval from the onset of symptoms until specimen collection is the most important determinant of the sensitivity of a biochemical marker.*If the patient history does not lend itself to documentation of an exact time of symptom onset it would be prudent to use the time interval from presentation to the ED to minimize ambiguity about the timing of blood samples for biochemical marker testing.
A reasonable period of observation is crucial to effectively rule out the possibility of AMI. The Emergency Medicine Cardiac Research Group Study[42] reported that AMI patients with non diagnostic ECGs present to the ED about 3 hours after symptom onset. They also report that from the fourth to ninth hour following symptom onset the sensitivity of CK-MB mass increased from >50% to >90%, and that between the eleventh and twelfth hour after symptom onset all chest discomfort patients with AMI had positive CK-MB determinations. A subsequent study[54] reported that the median duration of chest discomfort prior to ED presentation was 4 hours (range 2-9) and the interval from symptom onset to CK-MB elevation was 6 hours (range 4.3-9). This study also validated their earlier findings regarding sensitivity of CK-MB mass. From this and other studies[55,32] the guideline team concludes that a 12 hour observation period from symptom onset with serial CK-MB mass is a safe and cost effective strategy to rule out MI in intermediate risk patients.
RECOMMENDATION The guideline team recommends that the observation period for intermediate risk patients suspected of having possible unstable angina or an acute MI should be for 12 hours following onset of symptoms with CK-MB Mass testing every 3 hours from presentation. However, if the patient presents to the ED 6 hours after onset of pain then only an additional 6 hours of observation and testing prior to ETT is necessary. If the patient presents within 1 hour of symptom onset, then 12 hours of observation is recommended. This testing strategy should have sensitivity and specificity greater than 95% and approaching 100% based on a synthesis of our review. Furthermore, in borderline cases where there is reason to suspect a false positive elevation in CK-MB, or for patients who present with symptoms of possible ACS more than 24 hours after symptom onset, troponin 1 testing could be done to confirm the diagnosis. This strategy is safe, yet it represents a significant opportunity for reducing the length of hospital stay to evaluate MI compared to current practice (Strength of evidence = B).
EXERCISE TREADMILL TESTING
Although distinguishing between AMI and non-AMI patients in the ED setting is critical, of almost equal importance is determining which patients are truly having cardiac chest pain (angina) and those who are not. It is essential to diagnose angina accurately and to begin appropriate treatment immediately because these patients are at risk for a cardiac event in the near future.
RATIONALE FOR ETT Exercise treadmill testing (ETT) is favored because of its good sensitivity and specificity, its safety when used appropriately and its relatively low cost and wide availability[56]. Cardiac catheterization is considered the gold standard for detection of coronary artery disease but its invasiveness and cost preclude its use on all patients with chest pain. Thallium ETT and stress echocardiograms are more sensitive and specific than ETT but also require specialized personnel and are considerably more expensive. One of the key purposes of this guideline is to provide rapid and efficient disposition of these patients.
AVAILABILITY OF ETT
It is the opinion of the guideline team that seven day a week ETT availability within the facility should be the goal. Standard Bruce protocol ETT is the most widely used technique and the results must be immediately available.
PATIENT SELECTION AND TIMING OF ETT
Low risk patients can be discharged from the ED with an ETT to be done within 72 hours (preferably scheduled before the patient leaves the ED). The patient's primary physician should be apprised of any abnormal ETT results immediately. Intermediate risk patients should have an ETT before discharge from the ED unless they are admitted to the hospital.
Some patients have baseline ECG abnormalities (e.g., bundle branch block) or take medications (e.g., digoxin or betablockers) which will not allow standard interpretation of an ETT. However, performing an ETT on these patients may still provide useful clinical information as discussed below. Chronic antianginal medications should not be stopped in anticipation of an early ETT. Physical limitations and fixed rate pacemakers may preclude some patients from ETT entirely and these patients will require testing by another method, such as persantine thallium testing. If intermediate risk, these patients may require admission unless another form of testing is readily available. In these cases, a Medicine or Cardiology consultation is recommended to assist with the disposition of the patient.
INTERPRETATION Of ETT RESULTS
ETT results are usually reported as negative for ischemia, nondiagnostic (due to failure to achieve a desired workload of 85% of maximum predicted heart rate) or positive. Negative ETT results should allow discharge of the patient. Positive results must be interpreted in light of the clinical picture but generally these patients should be evaluated by an Internist or Cardiologist to determine final disposition. Certainly not all patients with abnormal results will need to be admitted but initiation of medical therapy and close follow-up is essential.
Patients with nondiagnostic ETT results are often the most difficult patients to manage. However, if the patient was able to achieve close to 85% maximum predicted heart rate or exercise for more than five metabolic equivalents (METS) without recurrence of his/her symptoms, the chance of a cardiac event in the near future is low[3]. Of course, the pre-test probability of cardiac disease is important and discussion with an Internist or Cardiologist should be considered.
ETTs done on women or patients on cardiac medications (such as digoxin)have a lower specificity but can still provide useful information regarding the risk of morbidity and mortality.
*Exercise treadmill testing (ETT) is favored because of its good sensitivity and specificity, its safety when used appropriately and its relatively low cost and wide availability.
*Low risk patients can be discharged from the ED with an ETT to be done within 72 hours (preferable scheduled before the patient leaves the ED).
*ETTs done on women or patients on cardiac medications (such as digoxin) have a lower specificity but can still provide useful information regarding the risk of morbidity and mortality.
*It is the consensus of the team that ETT is safe in intermediate risk patients after observation and testing as proposed in the accelerated evaluation protocol.
*One dose of non-enteric coated 325 mg (one adult tablet) or 162, mg (two baby tablets) of aspirin should be given to all patients except for those with clear-contraindications (allergy to aspirin).
SAFETY OF ETT ETT is very safe in low-risk patients[57]. The use of ETT in intermediate risk patients, especially those who have been observed as indicated in these guidelines appears to be safe. Since these patients have essentially been ruled out for MI, they are now in a lower risk category. Review of the literature did not uncover any published studies using this approach for intermediate risk patients, therefore evidence to support the safety is not available. Observational data from several centers using this approach have revealed no complications in low-risk patients. However, patients with unstable angina who have been inappropriately exercised have had serious complications[58] and it is therefore important to avoid ETT in patients who have high risk unstable angina. It is the consensus of the team that ETT is safe in intermediate risk patients after observation and testing as proposed in the accelerated evaluation protocol.
RECOMMENDATION Before leaving the ED, appropriate low risk patients should have an ETT scheduled within 72 hours, and the results should be communicated to the personal physician. Properly applied ETT is a useful tool in evaluating patients with intermediate risk once considered stable (Strength of evidence = Strong Consensus ).
OTHER TESTING
There is a subset of chest pain patients who are not suited for an ETT. Examples include those unable to walk on the treadmill, those with left bundle branch block and pacemaker dependent patients. Further evaluation of these patients may include nuclear or echo studies with exercise or pharmacological stress. Additional candidates for these alternate strategies are those with nondiagnostic, uninterpretable (e.g. digoxin, LVH. etc.) or inconclusive ETTs. It is unlikely that there will be sufficient demand for these alternate studies to warrant their immediate availability. Although the use of sestamibi or echocardiography for risk assessment in the Emergency Department has received significant attention and publicity over the last several years, their role in patients with unstable angina is ill-defined at this time and cannot be recommended.
TREATMENT DURING ACCELERATED EVALUATION PROTOCOL
Short stay or observation beds to be occupied by patients undergoing accelerated evaluation for acute coronary syndrome should be as well equipped as those in a step-down or transitional care unit. Blood pressure and continuous cardiac rhythm monitoring, suction, oxygen and resuscitation equipment and close proximity to nursing stations for easy observation by nursing personnel should be available.
The use of aspirin is generally well tolerated and may be helpful in decreasing mortality should the diagnosis of AMI or USA be eventually confirmed.[59] One dose of non-enteric coated 325 mg (one adult tablet) or 162 mg (two baby tablets) of aspirin should be given lo all patients except for those with clear contraindications (allergy to aspirin), The use of beta blockers in patients undergoing accelerated evaluation is not warranted.
If patients experience one or more episodes of chest pain during the period of observation, an ECG should be obtained and reviewed during the episode. If dynamic ST segment changes are found, the patient should be admitted to the ICU. Before nitroglycerin is administered, patients should be asked about recent sildenafil (Viagra ™) use as the combination of sildenafil and organic nitrates (nitroglycerin and nitroprusside products) can lead to severe and prolonged hypotension. It appears that patients will remain at risk for a serious drug interaction after administration of sildenafil for 24-72 hours, dependent upon patient age, renal and liver function. If there are no dynamic ST changes and the episode of pain lasts longer than 20 minutes despite nitroglycerin, the patient should be evaluated with biochemical marker testing every 3 hours.
SUMMARY & CONCLUSION
The evaluation of acute chest pain patients remains a complex challenge in the Emergency Department when the decisions to admit or discharge are based solely on traditional tools: the history, physical examination and ECG. Inevitably with such limited evaluation and disposition options, patients without acute ischemic heart disease may be unnecessarily admitted to scarce and expensive ICU/TCU beds, yet other patients with unrecognized acute coronary syndrome maybe discharged from the ED. Extensive review of the literature and expert opinion has resulted in this guideline group making the following observations:
* Initial clinical and ECG criteria can reliably stratify patients into high, intermediate and low risk of subsequent complications and/or death. High risk patients should he admitted because of the potential need for acute interventions. Low risk patients can be safely evaluated as an outpatient.
* For appropriately selected intermediate risk patients, an observation period including serial ECGs and biochemical markers will identify patients having more serious acute ischemic cardiac disease. For intermediate risk patients without chest pain lasting more than 20 minutes during the previous 24 hours, observation, serial ECG's and ETT before discharge is appropriate. Serial testing with biochemical marker is not required because these patients are unlikely to have had an infarction.
* Stabilized patients can safely undergo ETT. This will facilitate further risk stratification and will enable better admission and discharge decisions. A key feature of our recommendation is ready availability of ETT. The use of this accelerated evaluation protocol should begin in the emergency department and be the first step in an integratal approach to the management of patients who present with possible ACS. The optimal location for observing the intermediate risk patient should be situated in the ED. However, this may not be operationally feasible at some facilities and alternative sites may need to be identified. The use of this ED based protocol can assist in the more appropriate utilization of ICL/TCUs - i.e. decreased admission rates and shortened length of stays for patients subsequently found not to have acute coronary syndromes. The success of this model requires a multidisciplinary approach and interdepartmental cooperetion. The Emergency, Inpatient Critical Care, Lab, ECG and Nuclear Medicine Departments and their respective phyicians will need to collectively participate to ensure safe, efficient, cost-effective patient care.
REFERENCES
Young GY, Green TR. The role of single ECG, creatine kinase and CKMB in diagnosing patients with acute chest pain. Am J Emerg Hal 1993:11:444-9.
Goldiman I, Weinteg M, Weisbeig. M, Olshen R. Cook EF. Sargent RK, et al. A computer-derived protocol to aid in the diagnosis of emerency room patients with acute chest pain. N Eng Med 1982;307:588-96.
U.S. Department of Health and Human Services. Public Health Service. Agency for Health Care Policy and Research. Unstable angina; diagnosis and management.Washington, D.C.: USDHHS; 1994.
The Permanente Medical Group Department of Quality and Utilization. Unpublished Data; 1998
Roberts R, Kleinman NS. Earlier diagnosis and treatment of acute myocardial infarction necessitates the need for a "new diagnostic mind-set". Circulation 1994;89:872-81
A prospective trial of intravenous streptotinase in acute myocaidial infarclion (I.S.A.M.): Morbidity and Infaret Size at 21 Days. The I.S.A.M..Study Group. N Engl J Med1986;314:1465-71.
Effectivenes of intravenous thrombolytic treatment in acute myocardial infarction. Gruppo Italiano per lo Studio della Streptochinasi nelliInfarto Miocardico (GISSI). Lancet 1986;1:397-402.
Acute Myocardial Infarction, Clinical Practice Guideline. The Permanente Medical Group, October 1998.
Lee TH, Rouan G, Weisberg MC, Brand DA, Acampora D, Stasiulewicz C, et al. Clinical characteristics and natural histoiy of patients with acute myocardial infarction sent home from the emergency room. Am J Cardiol 1987:60:219-24.
Finebea HV, Sadden D, Goldman L. Care of patients with a low probability of acute myocardial infarction: cost effectiveness of alternatives to coronary-care-unit admission. NEnglJMed 1984:310:1301.7.
Bahr RD. Growth in chest pain emergency departments throughout the United States: a cardiologist's spin on solving the heart attack problem. Coron Artery Dis 1995:6:827-30.
Roberts RR. Costs of an emergency department-based accelerated diagnostic protocol vs. hospitalization in patients with chest pain: a randomized controlled trial. JAMA 1997;278:167-6
Rydnan R], Zalenski RJ, Roberts RR, Albrecht GA, Misiewicz VM Kampe LM, et al. Patient satisfaction with an emergency department chest pain observation unit. AnnEmergMed 1997;29:109-15.
Zalenski R), Rydlman RJ, McCarren M., Roberts RR,.Jovanovic B, Das K, et al. Feasibility of a rapid diagnostic protocol for an emergency department chest pain unit. Ann Emerg Med 1997;29:99-108.
Zalenski RJ, McCarren M. Roberts R, Rydman RJ.Jovanovic B, Das K, et al. An evaluation of a chest pain diagnostic protocol to exclude acute cardiac ischemia inthe emergency department. Arch intern Med 1997:157:1085-91.
Fesmire FM, Wears RL The utility of the presence or absence of chest pain in patients with suspected acute myocardial infarction. Am J Emerg Med. 1989.7(4): 372-377.
Lee TH, Rouan GW. Weisberg MC, Brand DA, Cook EF, Acampora D. et al. Sensitivity of routine clinical criteria for diagnosing myocardial infarction within 24 hours of hospitalization. Ann Intern Med 1987:106:181-6.
Yoseph R, Mervyn SG. The earliest diagnosis of acute mvocaidial infarction Annu Reve Med 1994;45:31-444
Solomon CG. Lee TH. Cook EF, Weishem MC, Brand DA. Rouan GJW, et al. Comparison of clinical presentation of acute myocardial infarction in patients older than 65 years of age to younger patients: the Multicenter Chest Pain Studv experience. Am J Cardiol 1989;63:772-6.
HerlitzJ.KarlsonBW.Lindqvist J, Sjolin M. Rate and mode of death during five years of follow up among patients with acute chest pain with and without history of diabetes mellitus. Diabet Med 1998;15:308-14.
Cunningham MA, Lee TH, Cook E, Biand DA, Rouan GW, Weisterg MC, et al. The effect of gender on the probability of myocaidial infarction among emergency department patients with acute chest pain: a report from the multicenter Chest Pain Study Group. J Gen Intern Med. 1989:4:392-8.
Heston TF, Lewis LM. Gender bias In the evaluation and management of acute nontraumatic chest pain. The St. Louis Emergency Physicians' Association Research Group. Fam Pract ResJ 1992;12:383-9.
HollanderJE, Todd KH, Green G, Heilpern KL. Karras DJ. Singer AJ, et al. Chest pain associated with cocaine: an assessment of prevalence in suburban and urban emergency departments. Ann Emer Med 1995;26:671-5.
Tokarski GF. Paganuss P. An evaluation of cocaine-induced chest pain. Ann Emerg Med 1990; 29: 1088-92.
McCarthy BD, BeshanskyJR. D'Agostino RB, Selker HP. Missed diagnoses of acute myocardial infarction in the emergency department: results from a multicenter study. AnnEmergMed 1993;22:579-82.
Fresmire FM, Percy FR, Wears RL, MacMath TL Risk stratification according to the initial electrocardiogram in patients with suspected acute myocardial infarction.Arch Intern Med 1989;149:1294-7. 27.
Roun GW, Lee TH, Cook EF, Brand DA, Weisberg MC, Goldman L Clinical characteristics and outcome of acute myocardial infarction in patients with initially normal or nonspecific electrocardiograms (a report from the Multicenter Chest Pain Study). Am J Cardiol 1989;64:1087-92.
Slater DK, Hlalky MA, Mark DB, Harrel FE Jr, Piror DB, Califf RM. Outcome in suspected acute myocardial infarction with normal or minimally abnormal admission electrocardiographic finding. Am J Cardiol 1987;60:766-70.
Bell MR, MontaTElloJK, Steel PM. Does the emergency room electrocardiogram identify patients with suspected myocardial infarction who are at low risk of Acute complications? AustNZ Med 1990:20:564-9.
BrushJEJr. Brand DA, AcamporaD.ChalmerB.WackersFJ. Use of the initial electrocardiogram to predict in-hospital complications of acute myocardial infarction. NEnglJMe 1985;312:ll37-41.
Lee TH, Cook EF. Weisberg MC, Rouan GW, Brand DA, Goldman L Impact of the availability of a Prior electrocardiogram on the triage of the patient with acute chest pain. JGen Intern Med 1990;5:381-8.
Goldman L, Cook EF, Johnson PA, Brand DA, Rouan GW, Lee TH. Prediction of the need for intensive care in patients who come to emergency departments with acute chest pain. NEnglJMed 1996;334:1498-1504.
Effects of tissue plasminogen activator and a comparison of early invasive and conservative strategies in unstable angina and non-Q-wave myocaidial infarction. Results of the TIMI IIIB Trial. Thrombolysis in Myocardial Ischemia. Circulation 1994 Apr;89(4):1545-1556.
Sekler HP, Zalenski RJ, Antman EM, Aufderheide TP, Bernard SA, BonowRO.et al. An evaluation of technologies for identifying acute cardiac ischemia in the emergency department: a report from a National Heart Attack Alert Program Working Group. AnnEmerMed l997;29:13-87
Wu AH, WangXM. Gornet TG.Ordonez-LlanosJ. Creatine kinase MB isoforms in patients with skeletal muscle injury: ramifications for early detection of acute myocardial infarction. Clin.Chem. 1992;38:2396-400.
Lee TH. Weisberg MC, Cook EF, Daley K, Brand DA, Goldman L. Evaluation of creatine kinase and creatine kinase-MB for diagnosing myocardial infarction: clinical impact in the emergency room. Arch Int. Med 1987;l47:115-21.
Hedges JR, Rouan GW, Toltzis R, Goldstein-Wayne B, Stein EA. Use of cardiac enzymes identifies patients with acute myocardial infarction otherwise unrecognized in the emergency department. Ann EmergMed 1987;16:248-52.
Irvin RG, Cobb FR, Roe CR. Acute myocardial infarction and MB creatine phosphokinase: Relationship between onset of symptoms of infarction and appearance and disappearance of enzyme. Arch Intern Med 1980:140:329-34.
Quale J.KimmelstielC,LipschikG,SchremS. Use of sequential cardiac enzyme analysis in stratification of risk for myocardial infarction in patients with unstable angina. Ann Intern Med 1988; 148:1277-9.
Lee TH, Cook EF, Weisberg M, Sargent RK. Wilson C, Goldman L. Acute chest pain in the emergency room: identification and examination of low-risk patients. Ann Intern Med 1986;145 65-9 41.
Lee TH, Goldman L Serum enzyme assays in the diagnosis of acute myocardial infarction: Recommendations based on a quantitative analysis. Ann intern Med 1986; 105:221-3.
Gibler WB, Young GP. Hedges JR, Lewis LM, Smith MS, Carleton SC, et al. Acute myocardial infarction in chest pain patients with nondiagnostic ECGs: Serial CK-MB sampling in the emergency department. The Emergency Medicine Cardiac Research Group. Ann EmergMed 1992;21:504-12.
TuckerJF, Collins RA. Anderson AJ, Hess M, Farley IM. Hagemann DA, et al. Value of serial myoglobin lewis in the early diagnosis of patients admitted for acute myocardial infarction. Ann Emerg Med 1994;24:704-8.
WooJ, Lacbawan FL, Sunheimer R, LeFever D. McCabeJB. Is myoglobin useful in the diagnosis of acute myocardial infarction in the emergency department setting? AnnJ Clin Palhol 1995;103:725-9.
Bakker AJ, GorgelsJPM, van Vlies B, Haagen FD, Smits R. The mass concentrations of serum troponin T and creatine kinase MB are elevated before creatine kinase and creatine kinase-MB activities in acute myocardial infarction. EurJCim Chem Clin Biochem 1993;31:715-24.
Ohman EM, et al. Cardiac troponin T levels for risk stratification in acute myocardial ischemia. GUSTO IIA Investigators. NEngljMed 1996;335(18):1333-134l.
Antman EM, et al. Cardiac-specific troponin I levels to predict the risk of mortality in patients with acute coronary syndromes. NEngl J Med l996;335(18):1342-9.
Christenson RH. Cardiac markers in the assessment of acute coronary syndromes proceedings from the 1st Maryland Chest Pain Center Research Conference. MdMedJ 1997;Suppl. 49.
Gibler WB, el al. Myoglobin as an early indicator of acute myocaidial infarction. Ann EmergMed 1987 (8):851-6. 50.
1998 Care Management Institute Survey of Kaiser Permanente Nationwide.
HammCW.et al. Emergency room triage of patients with acute chest pain by means of rapid testing for cardiac troponin T ortroponini. NEngl Med 1997;337(23):l648-l653.
Sayre MR, et al. Measurement of cardiac troponin T is an effective method for predicting complications among emergency department patients with chest pain.Ann Emerg Med 1998(5):539-549. 53
Personal communication: Ted Kutz,PhD, Director of Clinical Chemistry, University of California. San Francisco.
Young GP, et al. Serial creatine kinase-MB results are a sensitive indicator of acute myocardial infarction in chest pain patients with nondiagnostic electrocardiograms: the second Emergency Medicine Cardiac Research Group Study. AcadEmerg Med 1997(9):869-77.
Gibler WB, et al. A rapid diagnostic and treatment center for patients with chest pain in the emergency department Acad Emerg Med 1995(l):l-8.
Goldschlager N, Sefar A, Coin K. Treadmill stress tests as indicators of presence and severity of coronary artery disease. Ann Intern Med 1976:85:277.
Lewis WR, AmsterdamEA. Utility and safely of immediate excercise testing of low-risk patients admitted to the hospital for suspected acute myocardial infarction. Am J Cardiol 1994:74:987-90.
Personal communication: Ralph Brindis, MD and Michael Petru, MD, Cardiology Kaiser Permanente Medical Center, San Francisco.
Randomised trial of intravenous streptokinase, oral aspirin, both, or neither among 17,187 cases of suspected acute myocardial infarction: ISIS-2. ISIS-2 (Second Inimialional Study of Infarct Survival) Collaboratie Group. Lancet 1988;2:349-60.BACK to Kaiser Diagnostic and Treatment Documents Index